Uterine Fibroid Treatment in Goregaon West, Mumbai by Expert Gynecologist
Dr. Dimple Doshi (MBBS, MD, DGO)
Lady Gynecologist & Laparoscopic Surgeon
27+ years’ experience
20,000+ surgeries completed
Are heavy periods, large clots, pelvic pain, or constant bloating disrupting your daily life?
Do you feel drained, anxious, or embarrassed because of excessive bleeding or repeated emergency visits?
Are infertility struggles, miscarriages, or difficulty conceiving causing emotional stress and uncertainty?
Have you been searching for a safe, scientific, fertility-friendly treatment option that truly works?
When fibroids grow silently, they can take control of your life—causing anemia, severe cramps, back pain, pressure on the bladder, and even affecting your confidence due to a swollen lower abdomen. Many women begin avoiding travel, social events, intimate moments, and even work commitments because their symptoms feel unpredictable and overwhelming.
Here’s the good news: Fibroids are treatable. With the right diagnosis and personalized plan, you can finally reclaim comfort, energy, and fertility. At Vardaan Hospital, Goregaon West, Dr. Dimple Doshi (MD DGO)—a specialist in 3D Laparoscopic Myomectomy, fertility-preserving fibroid surgery, and advanced women’s health care—offers safe, minimally invasive solutions tailored to your symptoms, FIGO type, age, and fertility goals.
Your treatment may include medications, HIFU, UAE, or 3D laparoscopic/hysteroscopic myomectomy, planned with precision to restore your health and protect your uterus whenever possible.
Global & Indian Stats (AAGL / ISGE / Fertility & Sterility / Indian Data)
- 70–80% of women develop fibroids by age 50, but only 30% require treatment (AAGL).
- Submucosal and large intramural fibroids are linked to a 2–3× higher risk of miscarriage and 2–3% of infertility cases (Fertility & Sterility).
- Indian studies show 1 in 3 women above 30 have clinically significant fibroids, especially in the 30–45 age group (Indian JOG Research).
- Minimally invasive myomectomy (laparoscopic/hysteroscopic) offers faster recovery, minimal scars, and fertility preservation (ISGE 2024).
Sources:
AAGL – https://www.aagl.org
ISGE – https://www.isge.org
Fertility & Sterility – https://www.fertstert.org
What Are Uterine Fibroids?
Uterine fibroids are benign (non-cancerous) smooth-muscle tumors that grow within or around the uterus. They develop from the uterine muscle wall (myometrium) and vary in size—from tiny, seed-like nodules to large masses that distort the uterus.
Although not dangerous, fibroids can lead to heavy menstrual bleeding, painful periods, pelvic pressure, constipation, frequent urination, infertility, and recurrent pregnancy loss depending on their size and location.
Certain types—especially submucosal and large intramural fibroids—can directly affect fertility by interfering with implantation or distorting the uterine cavity.
Synonyms of Uterine Fibroids
- Fibroids
- Leiomyoma
- Myoma
- Uterine Myoma
- Fibromyoma
- Fibroid Tumor (Benign)
- Uterine Growth
- Fibroid Uterus
- Uterine Leiomyoma
- Uterine Mass
- Myomatous Uterus
What Are the Most Common Symptoms of Uterine Fibroids?
Uterine fibroids can cause heavy bleeding, pelvic pain, pressure symptoms, and fertility issues depending on their size, number, and location.
Bleeding-Related Symptoms
- Heavy menstrual bleeding
- Passing clots or sudden “flooding”
- Long or prolonged periods
- Iron-deficiency anemia
Pain & Pressure Symptoms
- Pelvic cramping or fullness
- Lower backache
- Abdominal heaviness
- Constipation due to bowel pressure
- Frequent urination from bladder compression
Reproductive & Fertility Symptoms
- Difficulty conceiving (infertility)
- Recurrent miscarriage
- IVF failure or poor implantation
- Higher risk of preterm labour
- Higher risk of malpresentations
Expert Tip — Dr. Dimple Doshi:
Early evaluation helps determine whether your symptoms are fibroid-related and if minimally invasive treatment is recommended.
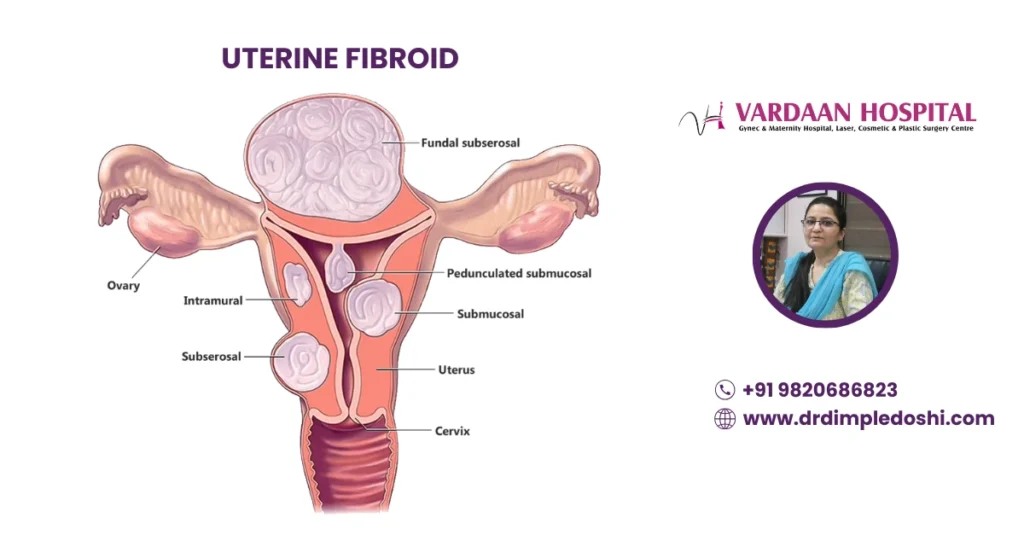
What Are the Different Types of Uterine Fibroids?
Fibroids can grow within the muscle, inside the cavity, on the surface, or on a stalk—each causing different symptoms, pressure effects, or fertility issues.
Types of Uterine Fibroids (Anatomical Classification)
1. Intramural Fibroids
- Grow within the uterine muscle wall
- Commonly cause heavy bleeding
- May affect fertility due to cavity distortion
2. Submucosal Fibroids
- Protrude into the uterine cavity
- Highest risk of infertility and miscarriage
- Can cause severe heavy bleeding
3. Subserosal Fibroids
- Grow outward from the uterus
- Cause bowel or bladder pressure
- Usually less associated with heavy bleeding
4. Pedunculated Fibroids
- Attached by a stalk
- Can twist and cause sudden, severe pelvic pain
5. Cervical Fibroids
- Develop in the cervix
- Can affect bladder, bowel function, and labour
6. Broad Ligament Fibroids
- Grow in the broad ligament beside the uterus
- Mimic ovarian cysts
- Cause pelvic pressure or fullness
What Is the FIGO Classification System for Uterine Fibroids?
The FIGO 0–8 system classifies fibroids based on their position in the uterus, helping guide treatment, fertility planning, and surgical approach.
FIGO 0–2: Submucosal Fibroids
- FIGO 0: Pedunculated intracavitary
- FIGO 1: <50% intramural
- FIGO 2: ≥50% intramural
Highest impact on heavy bleeding, implantation, and miscarriage.
FIGO 3–4: Intramural Fibroids
- FIGO 3: Touches endometrium
- FIGO 4: Completely intramural
May cause pain, heavy periods, and fertility disruption depending on size.
FIGO 5–7: Subserosal Fibroids
- FIGO 5: ≥50% intramural
- FIGO 6: <50% intramural
- FIGO 7: Pedunculated subserosal
Often cause pressure on bladder/bowel with less impact on periods.
FIGO 8: Other Locations
- Cervical
- Broad ligament
- Parasitic
These can mimic ovarian masses and require expert surgical evaluation.
Expert Insight — Dr. Dimple Doshi:
Understanding FIGO type ensures personalised treatment—especially crucial when preserving fertility or choosing minimally invasive surgery.
What Causes Uterine Fibroids to Develop?
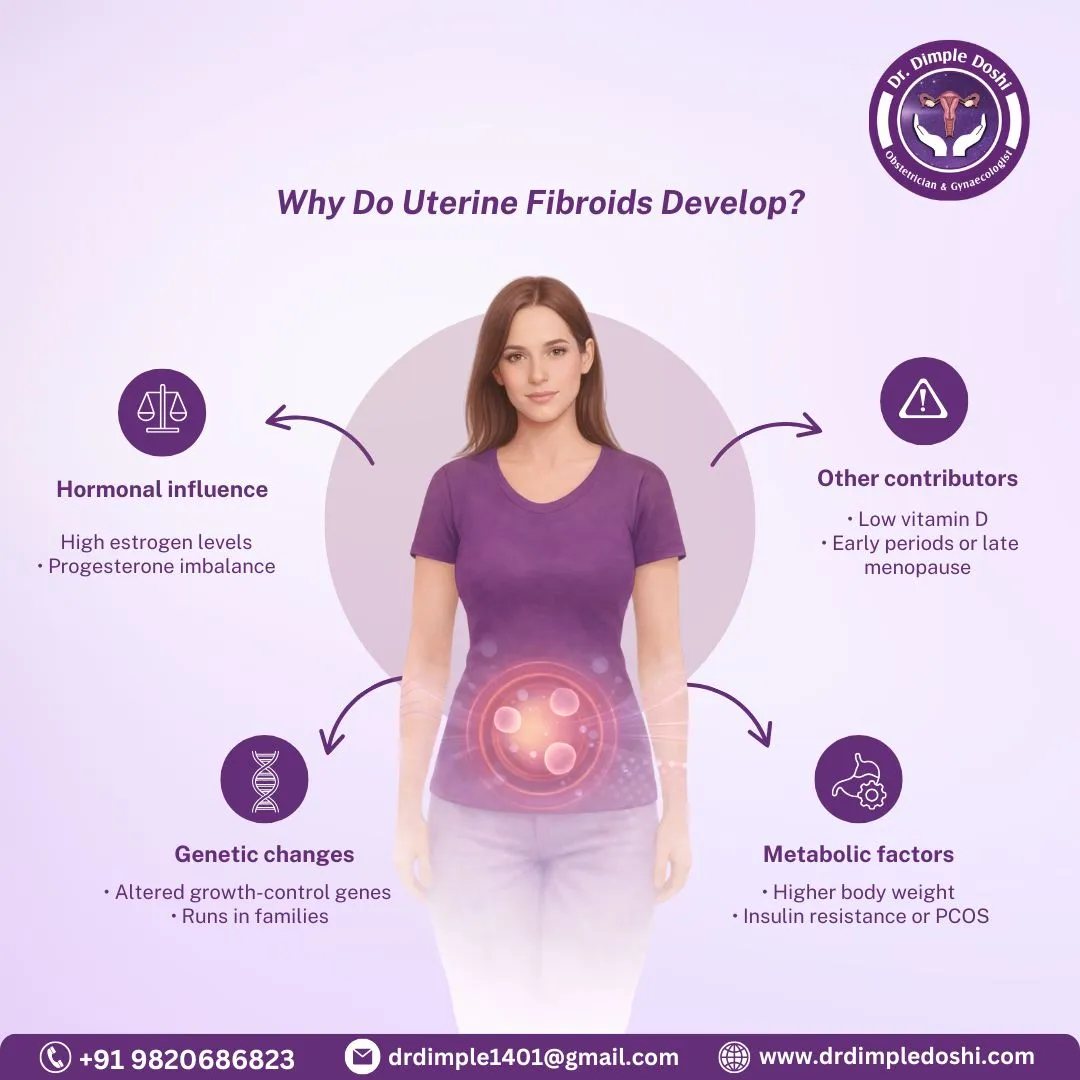
Fibroids form due to hormonal imbalance, genetic mutations, metabolic issues, and family or lifestyle factors that influence uterine muscle growth.
Hormonal Factors
- High estrogen levels
- Elevated progesterone
- Estrogen-dominant menstrual cycles
Genetic Mutations
- MED12 mutation
- HMGA2 mutation
These mutations are commonly seen in fibroid tissue.
Metabolic Factors
- Higher BMI
- Insulin resistance
- PCOS (polycystic ovary syndrome)
Other Contributing Factors
- Vitamin D deficiency
- Family history of fibroids
- Early onset of periods
- Late menopause
Expert Insight — Dr. Dimple Doshi:
Understanding the root cause helps tailor medical or surgical treatment—especially in women planning pregnancy or managing recurrent symptoms.
Who Is at Higher Risk of Developing Uterine Fibroids?
Women with hormonal imbalance, family history, higher BMI, PCOS, or early estrogen exposure have a greater risk of developing uterine fibroids.
High-Risk Groups for Uterine Fibroids
- Women aged 25–45
- Those with a positive family history
- Women with PCOS
- Overweight or higher BMI individuals
- Nulliparous women (no childbirth)
- Women of African ethnicity
- Those with Vitamin D deficiency
- Early menarche or prolonged estrogen exposure
Expert Insight — Dr. Dimple Doshi:
Identifying risk factors early allows timely screening and personalised treatment, especially for women planning pregnancy or experiencing heavy periods.
How can fibroids be prevented?
Fibroids can’t always be prevented, but maintaining hormonal balance, healthy weight, Vitamin D levels, and regular check-ups can lower risk and slow growth.
Ways to Reduce Fibroid Risk & Slow Their Growth
1. Maintain a Healthy Weight
- Less body fat = lower estrogen production
- Helps prevent hormonally driven fibroid growth
2. Correct Vitamin D Deficiency
- Vitamin D slows fibroid cell proliferation
- Supplementation helps high-risk women
3. Manage PCOS & Insulin Resistance
- Balanced hormones reduce fibroid trigger pathways
- Supports regular ovulation and metabolic health
4. Follow an Anti-Inflammatory, Fiber-Rich Diet
- More fruits, vegetables, whole grains
- Lowers inflammation and helps regulate hormones
5. Avoid Excess Estrogen Exposure
- Limit unnecessary hormonal supplements
- Review medications with your gynecologist
6. Exercise Regularly
- Boosts metabolism
- Supports weight control and hormone balance
7. Go for Routine Gynecology Check-Ups
- Early detection
- Timely management prevents complications
Expert Insight — Dr. Dimple Doshi:
While fibroids cannot be fully prevented, lifestyle and hormonal optimisation play a major role in reducing risk—especially for women with PCOS, high BMI, or strong family history.
How Do Uterine Fibroids Affect Fertility and Miscarriage Risk?
Fibroids can disrupt implantation, blood flow, and uterine space, leading to infertility or miscarriage. Treatment often improves natural conception and IVF success.
How Fibroids Affect Fertility
- Distortion of the uterine cavity
- Poor implantation of the embryo
- Reduced blood flow to the endometrium
- Abnormal uterine contractions
- Rarely, blockage of fallopian tubes
How Fibroids Increase Miscarriage Risk
- Weak anchoring of the embryo
- Distortion of the gestational space
- Inadequate blood supply to support early pregnancy
Post-Treatment Fertility Benefits
- Higher chances of natural conception
- Improved IVF implantation and success rates
- Reduced risk of early pregnancy loss
Expert Insight — Dr. Dimple Doshi:
Targeted fibroid treatment—especially for submucosal or cavity-distorting fibroids—can dramatically restore fertility and reduce miscarriage risk.
How Are Uterine Fibroids Diagnosed?
Fibroids are diagnosed through ultrasound or MRI to map their size and location, supported by blood tests to assess anemia and hormonal balance.
Key Diagnostic Tests for Fibroids
1. Transvaginal Ultrasound
- First-line test
- Detects size, number, and basic location
2. 3D Ultrasound
- Best for detailed FIGO classification
- Essential for fertility assessment and surgical planning
3. MRI Pelvis
- Used for multiple, deep, or complex fibroids
- Helps differentiate adenomyosis or ovarian masses
4. Blood Tests
- CBC and iron studies for anemia
- Assess severity of bleeding-related symptoms
5. Hormonal Evaluation (If Needed)
- For suspected PCOS or endocrine disorders
- Helps identify contributing factors
Expert Insight — Dr. Dimple Doshi:
High-quality imaging—especially 3D ultrasound and MRI—ensures accurate mapping, which is crucial for safe, fertility-focused fibroid treatment.
What Are the Treatment Options Available for Uterine Fibroids?
Fibroid treatment includes medicines, non-invasive therapies like HIFU, minimally invasive UAE, and surgical options chosen based on symptoms, fertility plans, and fibroid type.
A. Medical Treatment (For Symptom Control)
- Tranexamic acid
- NSAIDs
- Combined hormonal pills
- Progesterone therapies
- LNG-IUS (hormonal IUD)
- GnRH analogues
- Vitamin D supplementation
- Iron therapy for anemia
B. Uterine Artery Embolization (UAE)
A minimally invasive procedure that blocks blood supply to fibroids, shrinking them over time.
Benefits:
- No incision
- Day-care procedure
- Works for multiple fibroids
- Faster recovery
Limitations:
- Not ideal for women planning pregnancy
- Post-procedure pain common
- Possible reduction in ovarian reserve
C. HIFU (High-Intensity Focused Ultrasound)
A completely non-invasive, scar-free option using focused ultrasound waves to shrink fibroids.
Benefits:
- No stitches
- No anesthesia
- Scarless
- Day-care procedure
Limitations:
- Works only for selected fibroid types
- Not recommended if planning pregnancy
- Shrinkage is gradual
- Limited centre availability
D. Surgical Options (Brief Overview)
- Hysteroscopic myomectomy — for FIGO 0–2 submucosal fibroids
- Laparoscopic myomectomy — for intramural or subserosal fibroids
- Laparoscopic hysterectomy — for women with completed family
Open surgery is preferred only when fibroids are very large, deeply placed, extend into the broad ligament, those with multiple surgeries where adhesions are likely; or when laparoscopy is medically contraindicated .
Expert Insight — Dr. Dimple Doshi:
At Vardaan Hospital, all fibroid surgeries are performed using the Karl Storz Rubina 4K 3D system, ensuring precision, safety, and faster recovery.
Which Is the Best Hospital for Fibroid Treatment in Goregaon West, Mumbai?
If you’re looking for safe, advanced, and fertility-focused fibroid treatment in Goregaon West, Vardaan Nursing Home is widely regarded as one of the most trusted centres. Led by Dr. Dimple Doshi (MD DGO) —a specialist in 3D laparoscopic myomectomy, hysteroscopic fibroid removal, and minimally invasive gynaecological surgery—the hospital provides comprehensive care for women with symptomatic fibroids.
Vardaan Nursing Home stands out because it combines:
- Advanced 3D laparoscopic technology for precise, fertility-preserving fibroid removal
- Hysteroscopic techniques for cavity-distorting submucosal fibroids
- Fertility-friendly treatment planning based on FIGO classification
- Ultrasound + diagnostic hysteroscopy-based evaluation for accurate mapping
- Minimal-scar, faster-recovery surgeries performed by an experienced surgeon
- Personalised care for women seeking relief from heavy bleeding, pain, and infertility
Whether you need medications, UAE, HIFU, or laparoscopic/hysteroscopic myomectomy, Dr. Dimple Doshi ensures your treatment is scientific, safe, uterus-saving, and tailored to your age, symptoms, and pregnancy goals.
Why Patients Prefer Vardaan Nursing Home
- NABH-quality protocols
- 20+ years of clinical experience
- Thousands of successful women’s health surgeries
- Conveniently located in Goregaon West, Mumbai
- High reviews for compassionate, personalised care
Who Is the Best Gynecologist Obstetricians for Uterine Fibroid Surgery in Goregaon, Mumbai?
Dr. Dimple Doshi is a leading 3D laparoscopic fibroid surgeon in Goregaon, known for fertility-preserving expertise, 27+ years’ experience, and 25,000+ surgeries.
Why Patients Choose Dr. Dimple Doshi for Fibroid Surgery
- Pioneer in 3D laparoscopic fibroid surgery
- 27+ years of clinical experience
- 20,000+ surgeries performed with high safety standards
- Specialist in fertility-preserving myomectomy
- Member of MOGS, IAGE, FOGSI, AFG
- Renowned for empathetic counselling and surgical precision
- Performs all advanced procedures at Vardaan Hospital, Goregaon West
Medical Codes for Uterine Fibroids
ICD-10 Codes (Diagnosis Codes for Uterine Fibroids)
Uterine fibroids fall under Leiomyoma of Uterus (D25):
- D25.0 – Submucous Leiomyoma of Uterus
- D25.1 – Intramural Leiomyoma of Uterus
- D25.2 – Subserosal Leiomyoma of Uterus
- D25.9 – Leiomyoma of Uterus, Unspecified
CPT / Procedure Codes (Fibroid Treatment Codes)
These codes are used for procedures depending on the treatment type:
1. Myomectomy (Fibroid Removal Surgery)
- 58140 – Myomectomy, excision of fibroid(s), 1–4 intramural/subserosal
- 58146 – Myomectomy, 5 or more fibroids
- 58545 – Laparoscopic myomectomy, 1–4 fibroids
- 58546 – Laparoscopic myomectomy, 5 or more fibroids
2. Hysteroscopic Fibroid Removal
- 58555 – Diagnostic hysteroscopy (for cavity mapping)
- 58561 – Hysteroscopic myomectomy (resection of submucosal fibroid)
3. Uterine Artery Embolization (UAE)
- 37243 – Uterine fibroid embolization (UAE)
4. HIFU (High-Intensity Focused Ultrasound)
(No universal CPT code; commonly billed as)
- 0071T – Focused ultrasound ablation of uterine fibroids
- 0072T – Additional lesion ablation
- Hysterectomy (if used for complex cases)
- 58150 – Total abdominal hysterectomy
- 58570 – Total laparoscopic hysterectomy
- 58571 – TLH with removal of tube/ovary (if needed)
Indian Coding (ICD-10 + Procedure Terminology)
In India, hospitals typically use:
Diagnosis
- D25 (Leiomyoma of uterus) series for all fibroids.
Procedure Codes (Common in Indian EMR systems)
- O41.1 – Laparoscopic Myomectomy
- O41.2 – Hysteroscopic Myomectomy
- O41.3 – Uterine Artery Embolization
- O41.4 – HIFU for Fibroid
(Note: Some private hospitals use their own internal coding aligned with ICD-10 & IRDA procedure lists.)
(FAQ's) Frequently Asked Question of Uterine Fibroids
Q1. Do all fibroids need treatment?
Ans: No. Only fibroids causing symptoms, heavy bleeding, pressure effects, or fertility issues require treatment.
Q2. Can fibroids cause infertility?
Ans: Yes. Submucosal and intramural fibroids can disrupt implantation, blood flow, and embryo development, affecting fertility.
Q3. Can fibroids cause miscarriage?
Ans: Yes. Fibroids that distort the uterine cavity increase miscarriage risk by affecting embryo anchoring and gestational space.
Q4. Can fibroids shrink naturally?
Ans: Some fibroids shrink after menopause due to lower estrogen, but they rarely disappear completely.
Q5. Are UAE and HIFU safe?
Ans: Yes, both are safe for selected women. However, they are not recommended for those actively planning pregnancy.
Q6. Which treatment is best if I want to conceive?
Ans: Myomectomy hysteroscopic for cavity fibroids and laparoscopic for intramural/subserosal—is the preferred fertility-preserving option.
Q7. How do I know which fibroid treatment is right for me?
Ans: A detailed ultrasound or MRI, along with a consultation, helps determine the safest and most effective treatment based on FIGO type, symptoms, and fertility plans.
